In this month’s article, we discuss the complex aspects of women’s health, the burden of disease and how High Street Medical focuses on providing women with the highest quality of care through holistic and evidence-based practice.
Understanding women’s health
When it comes to talking about women’s health, it is important to understand the different factors or what we call health determinants because collectively, they influence and impact the entirety of an individual’s health and wellbeing.
Determinants of health include:
- Socio-economic
- Community and social
- Education and childhood development
- Living and working conditions
- Environmental/ geographic location
- Physical
- Genetic
- Age-related components
- Individual and lifestyle factors
According to the Australian Institute of Health and Welfare, the burden of disease in females consists of nearly half (44%) being from cancer, musculoskeletal and cardiovascular disease.
In a recent study published in the Australian and New Zealand Journal of Obstetrics and Gynaecology, 1 in 4 women are suffering from endometriosis and 1 in 11 with adenomyosis. However, these statistics are likely to be much higher due to the lack of general understanding and knowledge that surround endometriosis and adenomyosis because of their complexity and limited research that is currently being conducted.

Reproductive and sexual health
Medical issues that arise in women’s reproductive health generally occur during their reproductive years and can cause long term impacts on their overall health and well-being. In Victoria, there are significantly high numbers of women living with reproductive health conditions such as endometriosis and polycystic ovarian syndrome that are not well known or understood, many women silently suffer from symptoms of these diseases that are left untreated. Menopause is another condition that is not well managed among women in Victoria. This is thought to be due to a common fear of stigmatisation and inequality according to the Victorian Department of Health. Many women feel they might be treated differently if they were to seek medical advice or present to their GP for testing. In doing so, this compromises their overall general and reproductive health.
The following facts encompass true statements regarding sexual and reproductive health:
- It is about wellbeing within the individual, and not the absence of disease
- It requires respect, equality, safety and freedom from judgement and prejudice always
- It is applicable throughout a person’s lifetime, regardless of age
- It is unfairly and commonly judged by people’s sex and gender normativity, sexual orientation, expectations, and power play

A key determinant in women’s health is the right to exercise their own reproductive choices. Having access to information and medical advice allows women to be supported and reduce the risk of future health complications. At High Street Medical, the practitioners provide woman-centred care, focusing on each woman’s needs; their care is individually orientated. Our practice embraces an approach to medical care that encompasses a woman’s right to their own values, desires, personal and social circumstances. We provide conventional and alternative treatment management options and believe that our approach to health care empowers, heals, protects, and supports each and every one of our patients.
Regular Health Checks for women
At High Street Medical, the GPs encourage all female patients to have the following routine checkups:
Cervical Screening Test (Pap smear)
A screening test we use to check for irregularities or changes in the cervical cells. It is important to do this test every 2 years and necessary if you are sexually active. Having this test regularly can prevent 90% of cervical cancers through early detection. If you have had the human papillomavirus (HPV) vaccine it is still recommended that you have regular pap smears. More information on cervical screening tests can be found here.
STI screening
Will be performed by completing a urine test and will be combined with your cervical screening test. STI screening tests for sexually transmitted infections such as chlamydia. Chlamydia affects female fertility and presents often with no symptoms which is why it is important to test for it regularly specifically if you had unprotected sex with one or more partners.
Pregnancy
Part of your regular health check-up includes testing for pregnancy which the GPs will discuss with you before testing. This will be performed via a urine or blood test. If you are planning to become pregnant, make an appointment with us to visit one of the doctors practising at HSMC for a preconception consult to receive expert advice. More information on pregnancy services offered can be found here.
Methods of contraception
If you are not currently planning a pregnancy, it is important for you and your partner to use contraception. There are many different methods of contraception to choose from, some may suit you better than others. It is also important to remember that male and female condoms are the only method of contraception that will protect you from sexually transmitted diseases. Discussing this with your partner is most important to practice safe sex.
The type of contraception you use is your decision and choice. Your GP can recommend the best method that suits your requirements and health needs.
Contraceptive options include:
- Condoms
- Combined oral contraceptive pill (the pill)
- Progestogen-only pill or also known as the ‘mini pill’
- Vaginal ring
- Diaphragm
- Hormone injection which is given every 12 months
- Contraceptive implant
- IUD

If you would like more information on different contraceptive options, please click here.
The burden of disease in women

Endometriosis
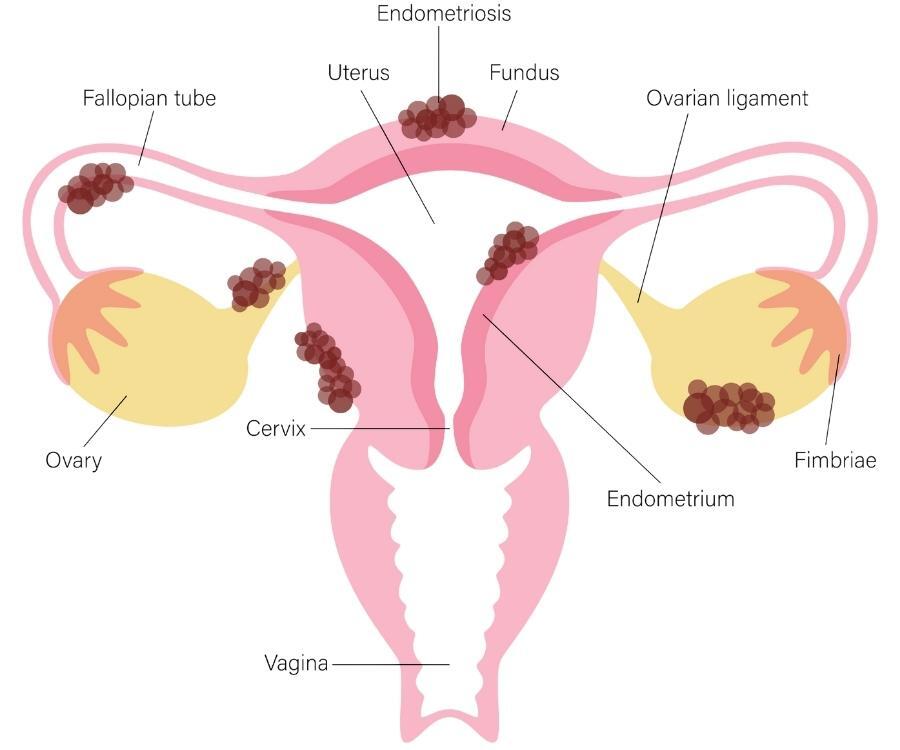
A painful and chronic condition that many Australian women are silently suffering with. The difficulty in diagnosis of endometriosis lies in the debilitating array of symptoms and early stages of the disease that cannot always be picked up on modern-day imaging, such as on ultrasound. Endometriosis should not be confused with period pain. It is a highly inflammatory disease that is caused when similar lining that grows inside the uterus grows outside the uterus, causing scar tissue. This tissue can grow on many organs, such as on the intestines, the bladder and even on the diaphragm.
Signs and symptoms
- Severe fatigue
- Brain fog
- Pain throughout your menstrual cycle or pain that continues all the time
- Pain during or after sexual intercourse
- Pain with bowel movements
- Pain when urinating
- Pain in the lower back or legs
- Frequency in urination and urgency
- Heavy or irregular periods
The 4 stages
It is not well known or understood that endometriosis actually presents itself in 4 different stages. These are graded from I-IV and can be classified by mild, moderate, or severe in state. These stages are defined below:
- Grade I (mild) stage presents internally as small scar tissue around the pelvic region
- Grade II (moderate) appears larger in size and scale in the pelvis cavity. It is at this stage that it has started to spread to the ovaries and significant adhesions can be seen
- Grade III-IV (severe) can be seen on all pelvic organs as well as the upper abdominal areas such as on the bowel
Diagnosis
A diagnosis of endometriosis can only be made through a biopsy of the endometrial tissue, which is taken via laparoscopy. This is a surgical procedure that is performed via keyhole surgery whilst under general anesthetic. Prospects of becoming pregnant need to be considered before undergoing this surgery as infertility risks can arise due to its invasiveness.
Treatment
Promoting awareness for endometriosis has never been so important because there is no cure for endometriosis which is why it is categorised as a chronic disease. There are treatment options that can alleviate symptoms but a woman who suffers from this debilitating disease will always feel the effects and unfortunately, the pain.
Currently, treatment options available include pain relief and anti-inflammatory medications as well as the contraceptive pill or IUD and surgical procedure. The natural rise and fall of estrogen and progesterone increase the presence of endometriosis and heightens related symptoms. Decreasing these natural hormones through the use of the contraceptive pill or IUD can help to reduce the presence of endometriosis. Surgical removal of endometriosis (endometrial ablation) is performed under general anaesthetic. Unfortunately, even with surgical removal of the endometrial tissue, the adhesions do grow back.
Other avenues of treatment include complementary medicine which has been known to reduce pain for many women with endometriosis. Physiotherapists, nutritionists and psychologists are able to provide these alternative treatments that help to alleviate the symptoms of endometriosis.
Adenomyosis
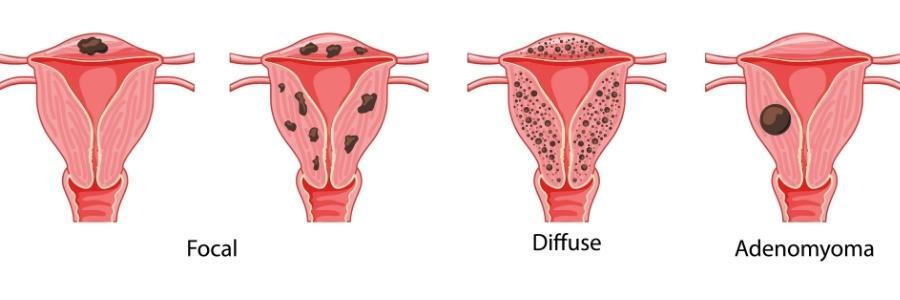
Adenomyosis is comparable to endometriosis where the same similar lining of the uterus grows elsewhere but instead of growing outside the uterus like endometriosis, the adenomyosis develops in the muscular wall of the uterus. Each menstrual cycle, it continues to increase in size and thicken which causes the uterus to become enlarged. This results in extreme pain and heavy periods. The concentration of adenomyosis growth in one area of the uterus muscular wall can cause a non-cancerous growth called adenomyoma as seen in the diagram above.
Signs and symptoms
- Pain during menstruation
- Heavy bleeding during menstruation
- Iron deficiency or anaemia
- Fatigue
- Dizzyness
- Pain during intercourse
- Chronic pelvic pain
- Tenderness and enlargement of the pelvic area
Risk factors
Unfortunately, not much is known about the causes of adenomyosis, however, certain risk factors have been a common similarity in women who have the disease. These include:
- Having a past history of uterine surgery, such as caesarean section, fibroid removal, or dilatation and curettage
- Childbirth
- Being middle-aged
Diagnosis
The uterus can present upon vaginal examination as enlarged or tender. Unfortunately, and similarly to endometriosis, adenomyosis can be tricky to diagnose because no test can confirm whether or not you have the disease unless the uterus is biopsied following a hysterectomy. A transvaginal ultrasound potentially may pick up adenomyosis as well as an MRI.
Treatment
There are 3 types of treatment options for adenomyosis. They consist of the following:
- Non-hormonal medication: Pain-relief, anti-inflammatory and antifibrinolytic medication
- Hormone treatments: IUD (Mirena) and contraceptive pill
- Surgical: a full hysterectomy which can be a very difficult decision for many women suffering from this debilitating disease
“Health is a state of complete physical, mental, and social well-being, and not merely the absence of disease or infirmity” – World Health Organisation
Discussing the importance of women’s health impacts all of us; it helps spread awareness of the burden of disease in women that desperately needs more research and attention. Our clinic is committed and dedicated to the health and well-being of all women.












